PurposeCurrently, the FDA allows biowaivers for Class I (high solubility and high permeability) and Class III (high solubility and low permeability) compounds of the Biopharmaceutics Classification System (BCS). Scientific evidence should be provided to support biowaivers for BCS Class I and Class III (high solubility and low permeability) compounds. MethodsData on the effects of excipients on drug permeability are needed to demonstrate that commonly used excipients do not affect the permeability of BCS Class III compounds, which would support the application of biowaivers to Class III compounds. This study was designed to generate such data by assessing the permeability of four BCS Class III compounds and one Class I compound in the presence and absence of five commonly used excipients. ResultsThe permeability of each of the compounds was assessed, at three to five concentrations, with each excipient in two different models: Caco-2 cell monolayers, and in situ rat intestinal perfusion. No substantial increases in the permeability of any of the compounds were observed in the presence of any of the tested excipients in either of the models, with the exception of disruption of Caco-2 cell monolayer integrity by sodium lauryl sulfate at 0.1 mg/ml and higher. ConclusionThe results suggest that the absorption of these four BCS Class III compounds would not be greatly affected by the tested excipients.
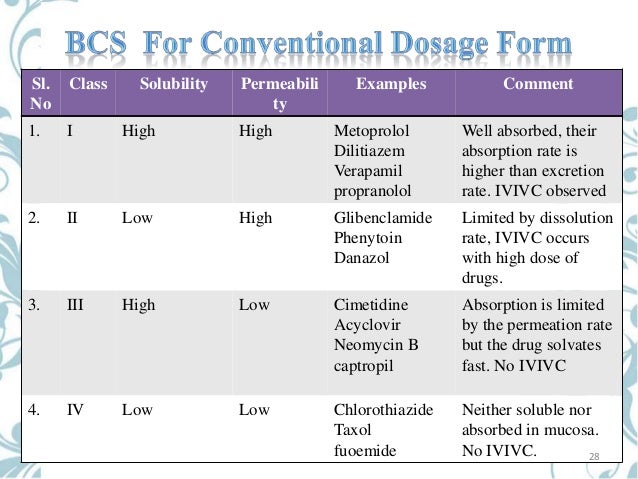
This may have implications in supporting biowaivers for BCS Class III compounds in general. The Biopharmaceutics Classification System (BCS) is a framework for classifying drug substances based upon their aqueous solubility and permeability across biological membranes. The FDA BCS guidance provides recommendations for sponsors of investigational new drug applications (INDs), new drug applications (NDAs), abbreviated new drug applications (ANDAs), and supplements to these applications (SNDA) who wish to request a waiver of in vivo bioequivalence (BE) studies for immediate-release (IR) solid oral dosage forms. Drug substances are classified based on their intestinal permeability (or the fraction of oral dose absorbed) and aqueous solubility at multiple pH values covering the range found in the gastrointestinal (GI) tract.
The solubility class boundary is based according to Papadopoulou et al. the highest dose strength of the drug substance in a pharmaceutical product that is dissolved in 250 ml (8 oz.) of aqueous buffer.Class I drugs have high permeability, and high solubility at all pH values between 1.0 and 7.5 (original FDA guidance from 2000), between 1.0 and 6.8 (new FDA draft guidance, May 2015) or between 1.2 and 6.8 (European Medicines Agency (EMA) and World Health Organization (WHO) (,); such compounds are well absorbed but may have poor bioavailability (BA) due to extensive first-pass metabolism. Class II compounds have high permeability, but their solubility is below the class boundary at one or more pH values (e.g., at low pH for acids or at neutral pH for bases).
The Biopharmaceutics Classification System (BCS) is the result of continuous efforts in mathematical analysis for the elucidation of the kinetics and dynamics of the drug process in the gastrointestinal tract (GIT) for NDA (New Drug Application) and ANDA (Abbreviated New Drug. Are bioWaiverS applicable for DrugS other than bcS claSS i? The US FDA currently accepts biowaivers only for BCS I, although Class III is under consideration. While scientifi c justifi cation may be considered for BCS II and III compounds in certain cases, these are not formally recognized under the current US BCS guidelines.
The fraction absorbed may be limited by their solubility; therefore, it is not uncommon to see a wide range of extent of absorption for this class of compounds. Class III drugs have low permeability and high solubility, and their fraction absorbed is sometimes limited by their permeability. Class IV drugs have both low permeability and low solubility.Class I drugs can be granted waivers from in vivo BE testing (“biowaivers”) due to their consistently high fraction absorbed, regardless of formulation. Several authors have suggested that Class III compounds should also be eligible for biowaivers if a new formulation does not change the permeability or the GI transit time of the drug (–). WHO recommends, and the new FDA draft guidance makes provision for, biowaivers for BCS Class III drug products, but only in cases where the generic and comparator drug products are very rapidly dissolving and the excipients meet certain criteria (e.g., qualitatively the same, quantitatively very similar, well-established for use in products containing that drug substance, do not affect GI motility or interactions with transport processes, and do not affect the pharmacokinetics (PK) of the drug substance) (,). This suggestion has also been proposed based upon a theoretical assessment of drug BA (,).Certain excipients have been shown either to enhance the in vitro permeability of drugs (e.g., by changing membrane integrity or affecting transporters) or to modify GI transit time (,).
Limited human data also suggest that some excipients may alter the BA of BCS Class III drugs (,). Several of these excipients have been demonstrated to alter membrane permeability directly, but others may work by inhibiting secretory transport mechanisms.In order to determine if a new formulation of a BCS III drug is suitable for a biowaiver, the potential effect(s) of the excipient(s) on permeability need to be evaluated. If no effect can be discerned in a well-validated in vitro model, it is reasonable to expect no change in permeability in vivo as well (–). First described for this purpose in 1989 , the utility of the Caco-2 cell monolayer model for qualitative (e.g., rank-order or high vs.
MaterialsGanciclovir was obtained from Toronto Research Chemicals (Toronto, Ontario, Canada). Acyclovir, antipyrine, atenolol, nadolol, digoxin, propranolol, d-glucose, d-lactose monohydrate, povidone K15, HPMC, PEG-400, SLS, 2-( N-morpholino)ethanesulfonic acid (MES), and Krebs Ringers buffer (KRB) were obtained from Sigma-Aldrich (St. Louis, MO, USA). Lucifer yellow (LY), Hanks’ balanced salt solution (HBSS), Dulbecco’s modified Eagle’s medium (DMEM), and 4-(2-hydroxyethyl)-1-piperazineethanesulfonic acid (HEPES) were obtained from Invitrogen (Carlsbad, CA, USA). Fetal bovine serum (FBS) was obtained from Omega (Tarzana, CA, USA). Penicillin, streptomycin, non-essential amino acids (NEAA), and trypsin-EDTA were obtained from CelGro (Herndon, VA, USA). Costar ® tissue culture flasks and dual-chamber Transwell ® plates were obtained from Corning (Corning, NY, USA).The excipients used and their respective concentrations are given in Table.
The selection of the excipients and the concentrations used in the study were based on information obtained from the FDA’s Inactive Ingredient Database. The inclusion criteria for selection of the excipient and the concentrations included the frequency at which the excipient is used (they are all commonly used), the amount of excipient typically used, the solubility of the excipient in physiological fluids, and the concentration of the excipient in the commonly used dosing volume of 250 ml. This may be an important factor in determining the choice of excipients in new formulations. BioanalysisA liquid chromatography–tandem mass spectroscopy (LC-MS/MS) analytical method was developed and validated for the simultaneous determination of the five compounds (acyclovir, antipyrine, atenolol, ganciclovir, and nadolol) in the presence of five excipients (HPMC, povidone, PEG-400, SLS, and lactose).
The analytical system was a PE SCIEX API 3000 LC-MS/MS with Flux Instruments Rheos 2000 pumps, a CTC Analytics autosampler, and an on-line degassing system. The LC column was a Thermo Aquasil C18 (3 μm, 50 × 2.1 mm) run at 300 μl/min with a 9-min gradient from 90% water/10% ammonium formate buffer (40 mM, pH 3.5) to 90% acetonitrile/10% ammonium formate buffer. Accuracy, based on analysis of replicate standards at 1 μM, was between 98.8 and 107% for all analytes, with coefficients of variation ranging from 2.6 to 5.9%.
Similar accuracy and precision were found at lower concentrations. Caco-2 CellsCaco-2 cells (clone C2BBe1) were cultured in DMEM supplemented with 10% FBS, 1 mM sodium pyruvate, 100 μM NEAA, 2 mM L-glutamine, 100 U/ml penicillin, and 100 μg/ml streptomycin. Stock cultures were grown in 175-cm 2 flasks at 37°C in a humidified atmosphere containing 5% CO 2. Cells were harvested with trypsin-EDTA, seeded at a density of 60,000 cells/cm 2 on collagen-coated Transwell plates (0.4-μm pore size), and grown at 37°C in a humidified atmosphere containing 5% CO 2. The culture medium was changed every other day for 10 days, and daily thereafter. Cell monolayers on Transwell plates were used for transport assays between 21 and 28 days post- seeding. Prior to use, each batch of monolayers was certified by measuring the transepithelial electrical resistance and the permeability of atenolol, propranolol, LY, and digoxin.
Permeability Across Caco-2 Cell Monolayers Non-specific Binding and Recovery AssessmentAcyclovir (100 μM), antipyrine (10 μM), atenolol (100 μM), ganciclovir (100 μM), and nadolol (100 μM) were dosed together as a cassette in the apical chamber of a cell-free Transwell device ( n = 3 replicates) to determine the non-specific binding (recovery) and cell-free apparent permeability across the membrane of each compound. Samples were collected from the donor and receiver chambers at multiple time points and analyzed by LC-MS/MS. “Cassette” refers to a small set of drugs (e.g., 3–5) or other compounds that are dosed together (co-dosed) for evaluation of their permeability ( in vitro), absorption ( in situ), or BA ( in vivo). The assumption is that they do not interact with each other or interfere with each other’s absorption, in which case the co-dosed results should reflect the results that would be obtained if they were dosed individually. Permeability AssayThe unidirectional (apical-to-basolateral (A→B)) and bidirectional (A→B and B→A) permeability of acyclovir, antipyrine, atenolol, ganciclovir, and nadolol, dosed as a cassette, was determined with Caco-2 cell monolayers.
Bidirectional permeability was measured in the absence of excipients only ( n = 3 replicates), whereas unidirectional permeability was measured both in the presence and absence of excipients ( n = 4 replicates). The transport buffer was HBSS, supplemented with 10 mM MES or HEPES buffer and 10 mM D-glucose (15 mM D-glucose final concentration). The pH of the buffer in the apical (A→B donor, B→A receiver) chamber was 6.8, and the pH of the buffer in the basolateral (A→B receiver, B→A donor) chamber was 7.4.
The apparent permeability (P app) and recovery were calculated as follows. LC-MS/MSThe LC-MS/MS method for acyclovir, antipyrine, atenolol, ganciclovir, and nadolol cassette analysis—in the presence and absence of the excipients HPMC, povidone, PEG-400, SLS, and lactose—had adequate sensitivity and selectivity and was valid for use in this study.
The lower limit of quantification (LLOQ) was 0.005 μM, and the upper limit of quantification (ULOQ) was 1 μM for all analytes. The intra- and inter-assay accuracy and precision were within ±12% of nominal at all concentration levels in all three matrices (HBSSg, pH 7.4; HBSSg, pH 6.8; and KRB, pH 6.8).
XNoticeThis website or its third-party tools process personal data (e.g. Hitachi seiki seicos manual free.
Benchtop, autosampler, and refrigerator stability were adequate, and no significant endogenous interference was found from HPMC, povidone, SLS, PEG-400, or lactose. Bidirectional PermeabilityAs shown in Table, all five compounds in the cassette had recoveries of at least 85% and high cell-free permeability under A→B test conditions. High recovery indicates little loss to either non-specific binding to the device or chemical instability during the assay, and high cell-free P appindicates that the compounds were freely diffusible across the membrane (lack of aggregation, etc.). The bidirectional permeability results presented in Table demonstrate that the BCS Class I compound antipyrine had much higher permeability across Caco-2 cell monolayers than the other four model compounds in the cassette (all of which were BCS Class III compounds), with complete recovery and no significant efflux (efflux ratio was approximately equal to 1). The permeability of acyclovir, atenolol, ganciclovir, and nadolol were each quite low and similar in magnitude to each other; the efflux ratios ranged from 2.1 to 2.7.
Unidirectional PermeabilityThe concentrations of the excipients tested are shown in Table. The concentrations (in mg/ml) are shown with the two permeability models, Caco-2 cells and rat intestinal perfusion.The results presented in Table demonstrate no consistent, concentration-dependent changes in the permeability of the model compounds across Caco-2 cell monolayers in the A→B (physiological absorptive) direction in the presence of up to 2.0 mg/ml lactose, 0.2 mg/ml povidone, 2.0 mg/ml HPMC, 0.04 mg/ml SLS, or 0.3 mg/ml PEG-400. The same was true for monolayer integrity (data not shown). On the other hand, SLS at concentrations of 0.1 and 0.17 mg/ml increased the post-experiment permeability of the monolayer integrity marker LY, indicative of damage to the cell monolayer (see footnote to Table ). The permeability of the model compounds in the presence of 0.1 mg/ml SLS was approximately 10-fold higher than control; permeability in the presence of 0.17 mg/ml SLS was not determined due to the evident cell monolayer damage.
Permeability in the Recirculating In Situ Rat Intestinal Perfusion ModelAs shown in Table and in Figs., and, the permeability results in the recirculating in situ rat intestinal perfusion model also suggest that lactose (up to 0.24 mg/ml), povidone (up to 0.06 mg/ml), HPMC (up to 0.06 mg/ml), SLS (up to 0.17 mg/ml), and of PEG-400 (up to 0.3 mg/ml) do not have a substantial effect on the permeability of the model compounds across rat jejunum. The small sample size precludes definitive conclusions regarding statistical significance. An LC-MS/MS method was validated for acyclovir, antipyrine, atenolol, ganciclovir, and nadolol determinations as a cassette in the absence and presence of excipients. This approach allowed for a relatively rapid assessment of the results of both arms of the study. This approach may be used to test the effects of other excipients on the same model compounds.The permeability of all five model compounds across intestinal epithelia was measured both in vitro (Caco-2 cell monolayers) and in situ (rat intestinal perfusion).
One problem with the intestinal perfusion model is that negative P eff values are often observed for low-permeability compounds. The most likely reason for a negative P eff value is that net water flux cannot be assessed accurately. When a small amount of a supposedly “impermeable” marker (FD-4 in this case, used to correct for water secretion) is absorbed, mathematically it results in overcorrection for water secretion, resulting in negative P eff values for low-permeability compounds. Currently, there are no perfect markers for the rat intestinal perfusion model.
FD-4 was used as the impermeable marker in this study, since this marker is widely accepted in the literature. Although negative P eff values for low-permeability compounds suggest that the rat perfusion model may be variable and potentially insensitive to small changes in drug absorption, this system is widely accepted for the evaluation of permeability.The permeability of the BCS Class I compound antipyrine across Caco-2 cell monolayers was high in both directions, with no asymmetry (ratio of B→A P app to A→B P app near unity).
The Caco-2 A→B (absorptive direction) permeability of the Class III model compounds acyclovir, atenolol, ganciclovir, and nadolol were all very low and nearly identical in magnitude (between 0.29 × 10 −6 and 0.32 × 10 −6 cm/s). The efflux ratios of the Class III compounds ranged from 2.1 to 2.7, a moderate degree of apparent efflux that is due in part to the fact that, in each case, the recovery was somewhat lower in the A→B direction than in the B→A direction, which would tend to underestimate the P app in the A→B direction (the denominator in the efflux ratio), leading to an overestimate of efflux. Clinically, linear peak plasma concentration as a function of oral dose (PK) has been reported for atenolol and nadolol (.
First generation antihistamine; an ethanolamine derivative. Uses for Doxylamine Succinate InsomniaSelf-medication for short-term management of insomnia, particularly in individuals who have difficulty falling asleep.Safety and efficacy not fully established; however, FDA states that, pending further accumulation of data, doxylamine-containing nighttime sleep aids approved for this use may continue to be marketed in the US. Nausea and Vomiting of PregnancyUsed in fixed combination with pyridoxine for treatment of nausea and vomiting of pregnancy in women not responding to conservative management.Not studied in patients with hyperemesis gravidarum. Allergic RhinitisTemporary relief of rhinorrhea, sneezing, lacrimation, itching eyes, or oronasopharyngeal itching associated with allergic rhinitis (e.g., hay fever) or other upper respiratory allergies. Doxylamine Succinate Dosage and Administration Administration Oral AdministrationAdminister orally as tablets.Delayed-release and extended-release tablets: Administer on an empty stomach with a glass of water.
Swallow whole; do not chew, crush, or split. DosageAvailable as doxylamine succinate; dosage expressed in terms of the salt.Also available as fixed-combination tablets containing doxylamine succinate and pyridoxine hydrochloride.Individualize dosage according to patient’s response and tolerance. Pediatric Patients Insomnia OralSelf-medication in children ≥12 years of age: 25 mg 30 minutes before retiring or as directed by a clinician.
Allergic RhinitisChildren 2 to 2 weeks. Specific Populations PregnancyCategory A.Doxylamine/pyridoxine in fixed combination intended for use in the management of nausea and vomiting of pregnancy. No increased risk of congenital malformations associated with the drugs reported in epidemiologic studies of pregnant women.Women considering self-medication with doxylamine during pregnancy should consult a health professional for advice regarding the relative risks and benefits of such therapy. LactationExpected to be distributed into milk.
Discontinue nursing or the drug. Do not use doxylamine/pyridoxine fixed-combination therapy in nursing women.Excitement, irritability, and sedation reported in infants presumably exposed to doxylamine through human milk; infants with respiratory syndromes (e.g., apnea) may be particularly at risk. Pediatric UseUse not recommended in premature or full-term neonates.Possible paradoxical excitement (e.g., restlessness, insomnia, tremors, euphoria, nervousness, delirium, palpitation, seizures).Safety and efficacy of doxylamine as a nighttime sleep aid in children.

